Polycystic ovaries: a common syndrome - AlloDocteurs
Polycystic ovary syndrome
One in ten women is affected by polycystic ovary syndrome. It is the most common hormonal abnormality in women of childbearing age. As it affects the ovaries and causes irregular and/or absence of ovulation, it often makes pregnancy more difficult to achieve.
The editorial staff of AlloDocteurs Written on , updated onWhat is polycystic ovary syndrome?
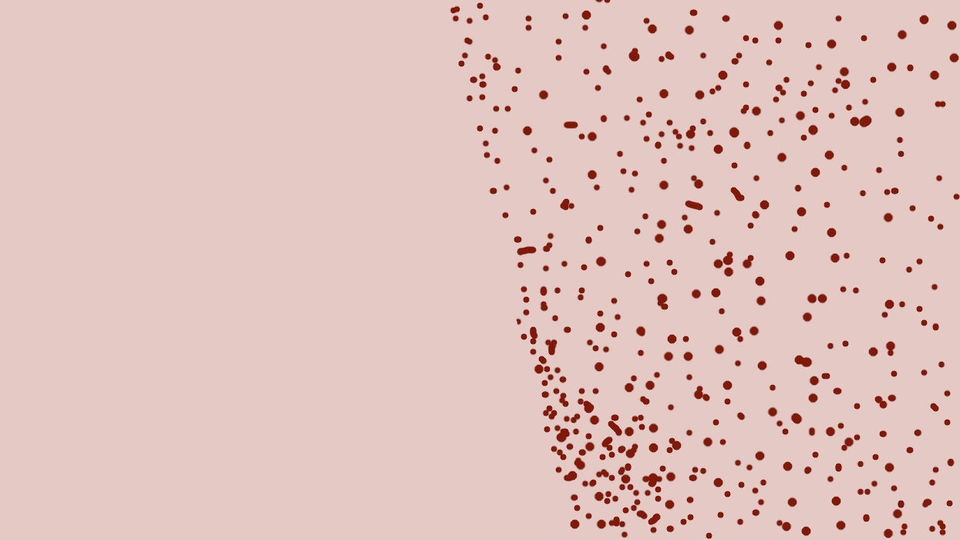
Polycystic ovary syndrome, also called "ovarian dystrophy", was discovered in 1935 by American researchers Stein and Leventhal.The ovaries are two essential glands for reproduction. They produce eggs, or oocytes, and release one each month: this is ovulation. Initially, the egg is a follicle. It must mature, that is to say finish its formation to lead to a mature egg. It then passes into the fallopian tubes and is eventually fertilized by a spermatozoon, if there has been sexual intercourse. At the time, and without an ultrasound, Stein and Leventhal thought that polycystic ovary syndrome was a multitude of cysts around ovaries, preventing ovulation. Thanks to ultrasounds, we have in fact realized that these are not cysts but follicles which do not reach maturity and which accumulate in the ovaries. The hormonal imbalance in question is probably due to genetic and environmental factors.
Polycystic ovary syndrome is characterized by an excess of male hormones. Periods are frequently irregular or even absent; in the most severe cases, there may be anovulation, i.e. the absence of egg production, but some women with the syndrome maintain normal ovulation or experience irregular ovulation
Excess male hormones can result in acne, increased body hair, oilier skin and hair. Weight gain, even obesity, is also common. These symptoms can occur from adolescence if the excess of androgens is important or the diagnosis is later, if the young woman tries to have a child and does not succeed.

The diagnosis is confirmed in the presence of 2 out of 3 associated symptoms: a cycle disorder (rareity of menstruation, irregular cycles sometimes lasting 30 or 40 days, irregular or absent ovulation), hyperproduction of male hormones responsible for acne and hyperpilosity or hirsutism, hair loss, and at least 12 large follicles per ovary, on ultrasound. More inconsistently, there may be anxiety, depressed mood, dark spots on the skin (called acanthosis nigricans). While the symptoms are well known, much is still unknown about the disease and its causes. A disorder of male sex hormones, obesity or a genetic origin would be involved. But there would be many other factors.
Many problems with polycystic ovary syndrome
Polycystic ovary syndrome persists throughout life. It has many problems that are not related to fertility. The amount of lipids, in other words fats, in the blood is often increased, which promotes cardiovascular disease. Obesity increases the risk of suffering from insulin resistance. It is indeed the first stage of type 2 diabetes, better known as fatty diabetes or adult-onset diabetes. Weight loss, which would reduce the risk of cardiovascular disease and diabetes, unfortunately seems more difficult to achieve in these patients. Mood disorders are also common.
The syndrome also increases the risk of endometrial cancer (source: INSERM), hence the importance of monitoring.
Diagnosis and treatment of polycystic ovary syndrome
The diagnosis is made through a blood test with a complete hormonal assessment (LH, FSH, androgens, possibly prolactin, testosterone, TSH), as well as a metabolic assessment evaluating blood sugar, cholesterol and triglycerides, possibly insulinemia (insulin level). Ultrasound shows at least 20 cysts, less than 9 mm in diameter and/or increased ovarian volume. Be careful, the ultrasound alone is not enough to confirm the diagnosis, some women presenting with follicles without other symptoms of PCOS.
Fortunately, many inconveniences can be significantly reduced with treatment tailored to each symptom and its intensity. The management is therefore personalized and some women will never need it because of very minimal symptoms. These treatments require the intervention of several doctors: medical endocrinologist, dermatologist, nutritionist, reproductive endocrinologist. They must be done over a long period, with regular monitoring.
Progesterone is given to regulate the cycles and reduce the signs of excess androgens (excess hair growth, acne, hair loss). If it is not sufficient, cyproterone acetate can be prescribed, in combination with an estrogen. Combined pills, combining estrogen and progestogen, also have an anti-androgenic effect. It is effective in 3 months on acne and 6 months on hirsutism.
Long-term hair removal is also an option to reduce hair growth.
Obesity requires diet rehabilitation, physical activity and sometimes psychotherapy. It is proven that a weight loss of at least 5% improves symptoms and promotes the restoration of ovulation. It also reduces the risk of developing type 2 diabetes (which will benefit from anti-diabetic medication per tablet if it occurs, and from an appropriate diet).
The care also depends on the desire for pregnancy. Hormonal stimulation based on clomiphene citrate or letrozole allows to restore ovulation and to be pregnant.
In case of failure, ovarian surgery by drilling can be proposed; this involves the practice of micro-perforations on the surface of the ovaries to restore ovulations and spontaneous pregnancies. The technique restores 50% of ovulations. As a last resort, in vitro fertilization is also a solution.
Learn more about ovarian cysts
Questions/answers:
And also:
Polycystic ovary syndromeOvariesGynecologyFertility, infertilityAbsence of periods